According to the National Health Commission website, since May 2022, monkeypox cases have been reported in many non-endemic countries around the world, and there is community transmission. In order to prepare for the medical response to monkeypox in advance and improve clinical early identification and standardized diagnosis and treatment capabilities, the National Health Commission and the State Administration of Traditional Chinese Medicine have formulated the "Monkeypox Diagnosis and Treatment Guidelines (2022 Edition)" (hereinafter referred to as "Diagnosis and Treatment"). guide").

The "Diagnosis and Treatment Guidelines" clarify the source of infection, transmission routes, susceptible groups, etc. of monkeypox. The full text is as follows:
Monkeypox Diagnosis and Treatment Guide
(2022 Edition)
Monkeypox is a zoonotic viral disease caused by infection with monkeypox virus (Monkeypox? virus, MPXV). The main clinical manifestations are fever and rash. , lymph node enlargement . The disease is mainly prevalent in Central Africa and West Africa. Since May 2022, monkeypox cases have also been reported in some non-endemic countries, and community transmission has occurred. In order to improve clinicians' ability to identify monkeypox early and standardize diagnosis and treatment, this diagnosis and treatment guideline is specially formulated.
1. Etiology
Monkeypox virus (MPXV) is classified into the genus Orthopoxvirus of the family Poxviridae, and is one of the four orthopoxvirus genera that are pathogenic to humans. The other three are smallpox virus , vaccinia virus and Vaccinia virus. Under the electron microscope , the monkeypox virus particles are brick-shaped or oval, 200nm × 250nm in size, and enveloped. The virus particles contain structural proteins and DNA-dependent RNA polymerase , and the genome is double-stranded DNA, which is about 197kb in length. Monkeypox virus is divided into two branches: the West African clade and the Congo Basin clade. The virus sequencing results of some cases in non-endemic countries this time are the West African branch. The main host of
monkeypox virus is African rodents (including African squirrels, tree squirrels, Gambian kangaroos, dormice, etc.).
Monkeypox virus is resistant to dryness and low temperatures and can survive for several months on soil, scabs, and clothing. Sensitive to heat, it can be inactivated by heating to 56°C for 30 minutes or 60°C for 10 minutes. Both ultraviolet rays and general disinfectants can inactivate it, and it is sensitive to sodium hypochlorite, chloroxylenol, glutaraldehyde, formaldehyde and paraformaldehyde.
2. Epidemiology
(1) Source of infection
The main source of infection is rodents infected with monkeypox virus. Primates (including monkeys, chimpanzees, humans, etc.) can also become sources of infection after infection.
(2) Transmission route
The virus invades the human body through mucous membranes and damaged skin. Humans are mainly infected through contact with the exudates, blood, and other body fluids of infected animals, or through bites or scratches from infected animals. Human-to-human transmission is mainly through close contact, but it can also be transmitted through droplets. It is also possible to be infected by contact with items contaminated with the virus. It can also be transmitted vertically through the placenta. Sexual transmission cannot be ruled out.
(3) Susceptible groups
people are generally susceptible. People who have been vaccinated with smallpox vaccine have a certain degree of cross-protection against monkeypox virus.
3. Clinical manifestations
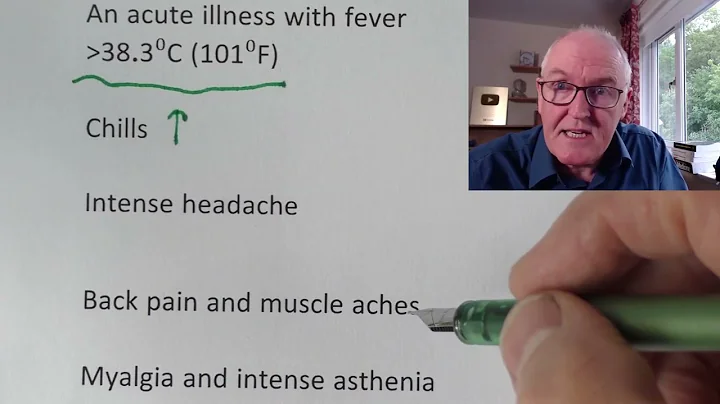
The incubation period is 5-21 days, mostly 6-13 days. Chills and fever appear in the early stage of the disease, and the body temperature is usually above 38.5°C, which may be accompanied by symptoms such as headache, drowsiness, fatigue, back pain, and myalgia. Most patients experience swollen lymph nodes in the neck, armpits, groin, etc.
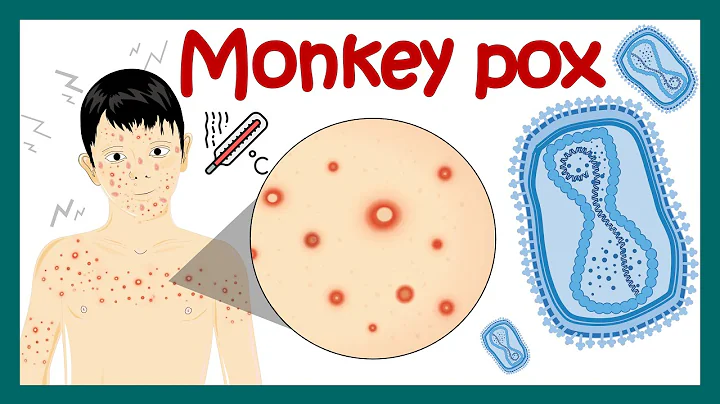
The rash appears 1-3 days after onset. The rash first appears on the face and gradually spreads to the limbs and other parts. The rash is mostly distributed centrifugally. Rashes on the face and limbs are more common than on the trunk. Rashes can appear on the palms and soles of the feet. The number of rashes ranges from a few to thousands. etc.; it can also involve oral mucosa, digestive tract, genitals, conjunctiva, cornea, etc. The rash goes through several stages from macules , papules, herpes, pustules to scabs. Herpes and pustules are mostly spherical, about 0.5-1 cm in diameter, with a hard texture and may be accompanied by obvious itching and pain.
It takes about 2-4 weeks from the onset of symptoms to the scabs falling off. After the scabs fall off, erythema, pigmentation, and even scars may remain, and the scars may last for several years. Some patients may develop complications, including secondary bacterial infection at the skin lesion, bronchopneumonia, encephalitis, corneal infection, sepsis, etc.
Monkeypox is a self-limiting disease, and most cases have a good prognosis. Severe cases are common in young children and people with low immune function. The prognosis is related to the branch of the virus infected, the degree of virus exposure, previous health conditions, and the severity of complications. The case fatality rate of the West African branch is about 3%, and the case fatality rate of the Congo Basin branch is about 10%.
IV. Laboratory examination
(1) General examination
peripheral blood white blood cells are normal or increased, platelets are normal or decreased. Some patients may experience elevated transaminase levels, reduced blood urea nitrogen levels, hypoalbuminemia , etc.
(2) Etiological examination
1. Nucleic acid detection : Monkeypox virus nucleic acid can be detected in specimens such as rash, blister fluid, scab, oropharyngeal or nasopharyngeal secretions using the nucleic acid amplification detection method.
2. Virus culture: Monkeypox virus can be isolated by collecting the above specimens for virus culture. Virus culture should be carried out in biosafety laboratories at level three or above.
5. Diagnosis and differential diagnosis
(1) Diagnostic criteria
1. Suspected cases
Those with the above clinical manifestations must also have any of the following epidemic histories:
(1) Areas where overseas monkeypox cases have been reported within 21 days before the onset of disease. Travel history;
(2) Close contact with monkeypox cases within 21 days before onset of illness;
(3) Contact with the blood, body fluids or secretions of animals infected with monkeypox virus within 21 days before onset of illness.
2. Confirmed cases
Suspected cases and monkeypox virus nucleic acid test is positive or monkeypox virus is isolated by culture.
For cases that meet the criteria for suspected cases or confirmed cases, infectious disease reporting should be carried out in accordance with relevant requirements.
(2) Differential diagnosis
is mainly distinguished from chickenpox, herpes zoster, herpes simplex, measles, dengue fever and other fever and rash diseases. It is also differentiated from skin bacterial infections, scabies, Identification of syphilis and allergic reactions.
6. Treatment
At present, there are no specific anti-monkeypox virus drugs in China. They mainly focus on symptomatic support and treatment of complications.
(1) Symptomatic and supportive treatment. Rest in bed, pay attention to replenishing nutrients and water, and maintain water and electrolyte balance. For those with high body temperature, physical cooling is the main method. If the temperature exceeds 38.5°C, antipyretic and analgesic drugs should be given to reduce the fever, but care should be taken to prevent excessive sweating from causing collapse.
Keep the skin, mouth, eyes, nose and other parts clean and moist, and avoid scratching the skin in the rash area to avoid secondary infection. Analgesics can be given if the pain at the rash site is severe.
(2) Treatment of complications. When secondary skin bacterial infection occurs, effective antibacterial drug treatment is given, and adjustments are made based on the culture, isolation, identification and drug sensitivity results of the pathogenic bacteria. Prophylactic use of antibiotics is not recommended. When corneal lesions occur, eye drops can be applied, supplemented by vitamin A and other treatments. When encephalitis occurs, treatment such as sedation, dehydration, lowering intracranial pressure, and airway protection are given.
(3) Psychological support treatment. Patients often suffer from psychological problems such as stress, anxiety, and depression. Psychological support, counseling, and related explanations should be strengthened. Psychological specialists should be consulted in a timely manner according to the condition and participate in disease diagnosis and treatment. If necessary, corresponding drug-assisted treatment should be provided.
(4) Traditional Chinese medicine treatment. Treatment is based on syndrome differentiation and treatment based on the principles of traditional Chinese medicine "examination of causes and treatment" and ", three causes and conditions". For those with clinical symptoms of fever, it is recommended to use Cimicifuga Gegen Decoction , Shengjiang Powder, Zixue Powder , etc.; for those with clinical symptoms of high fever, dense acne rash, sore throat, multiple lymph node swelling and pain, it is recommended to use Qingying Decoction , Shengjiang Powder Ma Biejia Decoction, Xuanbai Chengqi Decoction , etc.
7. Discharge criteria
Patients can be discharged if they meet the following criteria: body temperature is normal, clinical symptoms have improved significantly, and scabs have fallen off.
8. Infection prevention and control in medical institutions
Suspected cases and confirmed cases should be placed in isolation wards. Suspected cases are isolated in a single room.
Medical staff implement standard precautions, take contact prevention and droplet prevention measures, wear disposable latex gloves , medical protective masks, protective visors or goggles, disposable isolation gowns, etc., and also perform good hand hygiene.
strictly disinfects patients' secretions, feces and blood contaminants in accordance with the "Technical Specifications for Disinfection of Medical Institutions".
Source: Popular Science China



![2022 Monkeypox Outbreak | Everything You Need to Know [August 2022] - DayDayNews](https://i.ytimg.com/vi/M9eZvPwbvgE/hq720.jpg?sqp=-oaymwEcCNAFEJQDSFXyq4qpAw4IARUAAIhCGAFwAcABBg==&rs=AOn4CLDoXFkUIMsvbGZLccgUsCzfzjLt9g)