Cerebral hemorrhage is the stroke type with the highest disability and mortality rates, accounting for 20% to 30% of all cerebrovascular diseases. The acute phase mortality rate is 30% to 40%. It is one of the diseases that seriously endangers human health. . In order to have a deeper understanding of the clinical emergency of cerebral hemorrhage, Director Du Zhigang from Beijing Ditan Hospital has sorted out the key points of diagnosis and treatment of cerebral hemorrhage. Let’s learn together now.
Blood vessels that turn thousands of times - the complex blood supply system of the brain
Why cerebral hemorrhage occurs has to start with the anatomical structure of the complex tissue of the brain.
The arterial blood supply of the brain comes from: ① internal carotid artery system; ② vertebral-basilar artery system.

Internal carotid artery: The internal carotid artery enters the skull through the rupture hole, and the intracranial segment passes through the dura mater and passes through the cavernous sinus , and then branches out into the ophthalmic artery, posterior communicating artery, anterior choroidal artery, anterior cerebral artery. Artery (separates from the parachiasm), and its terminal branch is the middle cerebral artery. The internal carotid artery system supplies: blood flow to the front 3/5 of the brain including the frontal lobe, temporal lobe, parietal and basal ganglia, also known as the anterior circulation of the brain.
vertebral-basilar artery system: The bilateral vertebral arteries enter the skull and divide into the posterior inferior cerebellar artery, which travels to the pontine sulcus and merges into basilar artery , which in turn divides into the anterior inferior cerebellar artery, pontine branch, internal auditory artery, and cerebellum. Superior artery, to the interpeduncular fossa basilar artery divides into two left and right posterior cerebral arteries.
The two posterior cerebral arteries are circular upward, and send out multiple thalamic perforating branches, thalamic geniculate body perforating branches and posterior choroidal arteries. The cortical branches supply the base of the temporal lobe and occipital lobe of the brain.
The vertebrobasilar artery system supplies blood to the posterior 2/5 of the brain, including the brainstem, cerebellum, posterior part of the cerebral hemisphere and part of the diencephalon, also known as the posterior circulation of the brain.
The unbearable weight of blood vessels - the cause and pathogenesis
Normal cerebral arteries can withstand 150mmHg pressure without rupture. Long-term sustained hypertension will harden the small arteries in the brain, produce fatty hyalinization, and form micro aneurysms. , when blood pressure suddenly rises, blood vessels rupture and bleed.
There are many causes of cerebral hemorrhage, the common ones are as follows, among which hypertensive cerebral hemorrhage is the most common cause.
Common:
1. Hypertension, cerebral arteriosclerosis;
2. Congenital arterial vascular malformation or aneurysm, moyamoya disease ;
3. Blood diseases (leukemia, aplastic anemia , thrombocytopenia, hemophilia , etc.) ;
4. Anticoagulation or thrombolytic therapy and cerebral hemorrhage after infarction;
5. Amyloid angiopathy.
Rare causes include:
1. Cerebral arteritis , viral infection leading to necrosis and rupture of the vessel wall;
2. VitC and K deficiency, intimal necrosis of small blood vessels in the brain;
3. Primary or metastatic tumors.
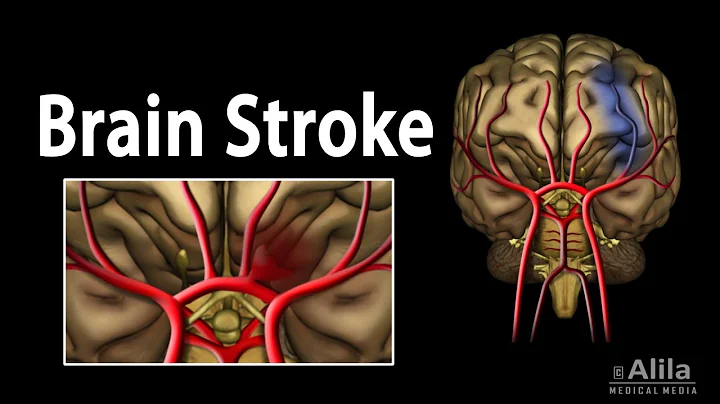
The arteries prone to cerebral hemorrhage are: (see the figure below for details)
·1. Branches of the middle cerebral artery → lateral branch of the lenticulostriate artery
·2. Branches of the posterior cerebral artery → thalamic perforating artery
·3. Branches of the posterior cerebral artery → thalamic geniculate artery
·4. pontine hemorrhage is a branch of the basilar artery → paramedian artery
·5. cerebellar hemorrhage → branch of the superior cerebellar artery
·6. intraventricular hemorrhage → veins Plexus vessel rupture


a mess - the pathology of cerebral hemorrhage
The vast majority of hypertensive ICH occurs most frequently in the putamen and internal capsule of the basal ganglia, accounting for about 70% of ICH. Followed by the thalamus, cerebral lobes, pons , cerebellum, ventricles , etc.

ICH symptoms are mainly caused by cerebral edema caused by local bleeding and hematoma formation in the brain tissue, and pressure, movement, softening, and necrosis of the brain tissue. The cerebral hemisphere on the bleeding side has obvious edema and swelling, which can cause the lateral ventricle to deform significantly and move to the opposite side. In severe cases, it can form cerebral herniation. Cerebral herniation is the most common direct cause of death of all types of cerebral hemorrhage.
The blood in the basal ganglia area ICH can break into the lateral ventricles and subarachnoid space . In lesions with recent hemorrhage, the brain tissue damaged by hemorrhage presents irregular cavities, which are filled with frozen liquefied blood. The cavities are surrounded by softening zones, which are caused by obstruction of local venous drainage due to hemorrhagic edema. More spotty bleeding.
After the acute phase, the blood clot melts, phagocytes remove hemosiderin and necrotic brain tissue gliosis, small bleeding lesions form glial scars, and large bleeding lesions form stroke cysts.

Positioning signs are very important, and there are skills to identify them at a glance.
Different bleeding sites may have certain unique symptoms and signs. Positioning signs can be used to determine the bleeding site during diagnosis and treatment.
1, Hemorrhage in the basal ganglia
This is a common site for hypertensive cerebral hemorrhage, accounting for 60% to 70% of ICH (putamen is the most common, accounting for 60%, thalamus 10%, caudate Core , ribbon core Rare) .
① Putamen hemorrhage: is the lateral type of the internal capsule, (rupture of the lenticulostriate artery) , and the hematoma presses inward near the internal capsule:
● Contralateral to the lesion Hemiplegia , hemi-sensory disorder and homonymous hemianopia ( Three partial) .
● Both eyes stare toward the lesion.
● Dominant hemisphere lesions may cause aphasia .
● Heavy bleeding may cause disturbance of consciousness.
If the bleeding volume in the basal ganglia area is 30ml, the condition is serious and very critical, and the following symptoms will occur:
● The onset is acute, the consciousness is severely disturbed, and coffee-like substance is vomited.
● central respiratory failure (Tidal style) .
● stress ulcer.
● The eyeball stares to the side of the lesion or the eyeball is fixed.
● hemiplegia, muscle tension ↓, pathological signs (+), when lying down, the affected limb is in an external rotation position.
● Cerebral herniation; mydriasis on the bleeding side, hemiplegia on the contralateral side, and central hyperthermia.
② Thalamus hemorrhage (rupture and bleeding of thalamic geniculate artery and perforating artery) : namely, lateral type of internal capsule, hematoma compresses the internal capsule outward:
● lesion contralateral hemiplegia, hemi-sensory disorder and homonymous hemianopia (three Partially) , the sensory impairment is more severe.
● When extends downward to the hypothalamus and midbrain , eyeball deviation, dissociative strabismus, upward vision disorder or staring at the tip of the nose will occur.
● Hemorrhage spreads to the hypothalamus or breaks into the third ventricle , with deepening disturbance of consciousness, miosis, cortical rigidity and other midline symptoms.
③ Hemorrhage in the head of the caudate nucleus
Symptoms of small amount of bleeding and easy rupture into the ventricle
● Headache, vomiting, and meningeal irritation (+).
● may have contralateral central tongue and facial paralysis.
● is similar to subarachnoid hemorrhage .
2. Lobar hemorrhage
is more common in the parietal lobe, followed by the temporal, occipital and frontal lobes, and can also involve several lobes at the same time.
• Most common in young people are vascular malformations and Moyamoya disease, with irregular hematoma edges and mixed density within the hematoma.
• Cerebral arteriosclerosis, amyloid angiopathy, tumors, etc. are more common in the elderly.
• Clinical manifestations depend on the location and amount of bleeding.
• Sudden headache, the degree of headache depends on whether the hematoma has penetrated.
• Related to the ventricles or subarachnoid space.
• May have hemiplegia, somatosensory disorder, and hemiplegic characteristics.
• The degree of monoplegia or upper and lower limb paralysis is inconsistent.
• There may be epilepsy, mental symptoms, incomplete aphasia, strong grasping, groping, visual impairment, meningeal irritation, etc.
Its characteristics can also be seen in different cerebral lobe hemorrhages:
● Frontal lobe - hemiplegia, motor aphasia (Broca), psychosis, groping, strong grasping, etc.
● Temporal lobe - visual hallucinations, auditory hallucinations , psychiatric symptoms, sensory aphasia (Wernicke), etc.
● Parietal lobe - hemibody sensory impairment , apraxia, body image disorder, etc.
● Occipital lobe — visual field defect or cortical blindness.
3, Brainstem hemorrhage
Mid-cerebral hemorrhage
Small amount of bleeding→ipsilateral or bilateral oculomotor nerve damage, abnormal eye position, accompanied by contralateral or bilateral pyramidal tract signs.
Massive bleeding → Deep coma , bilateral pupils were dilated, and immediate death.

Pontine hemorrhage: (rupture of the pontine branch of the basilar artery)
accounts for 10% and is a common site for brainstem hemorrhage. Symptoms include sudden headache, vomiting, dizziness, diplopia, side view paralysis, cross paralysis, and quadriplegia.
① Mild: bleeding <5ml
• Clear consciousness.
• When the lesion is located on the ventrolateral side, it shows abducens nerve paralysis and peripheral facial paralysis on the side of the lesion, contralateral limb paralysis and hemispheric sensory impairment. (Millard-Gubler syndrome).
● The base of the pontine is damaged: ( locked-in syndrome )
● shows eye level movement disorder, bilateral facial paralysis, tongue paralysis, articulation, swallowing movement disorders, quadriplegia, and positive pathological signs.The reticular activating system of the cerebral hemispheres and brainstem tegmentum is intact, and consciousness is clear. There may be high fever, profuse sweating, stress ulcers, myocardial ischemia, etc.
② Severe: bleeding >5ml
• Severe disturbance of consciousness.
• quadriplegia, a few may develop decerebrate ankylosing syndrome.
• The eyeballs float and the pupils shrink like pinpoints.
• vomits coffee-like stomach contents, has central high fever, irregular breathing, and usually dies within 24 to 48 hours.
Bulbar hemorrhage
Primary bulbar hemorrhage is rare. Most cases of pontine hemorrhage extend to and medulla oblongata , causing sudden coma, drop in blood pressure, irregular respiratory rhythm, and heart rhythm disorder, and rapid death.
4, small cerebral hemorrhage : accounting for 10%
is more common in the cerebellar hemisphere or the middle and outer parts of the cerebellum.
• Sudden dizziness, frequent vomiting, and severe headache in the back of the head.
• Ataxia on the lesion side, nystagmus .
• Those with large amounts of bleeding may suffer from coma, increased intracranial pressure , and death from foramen magnum hernia is very likely to occur.

5, intraventricular hemorrhage
Primary intraventricular hemorrhage (choroid plexus vessels)
• Headache and vomiting, Neck stiffness .
• Disorder of consciousness or transient disorder of consciousness.
• It is bloody, the amount of bleeding is small, and the prognosis is good.
• Patients with massive bleeding are in serious condition, comatose, have extremely small pupils, separated strabismus or floating eyeballs, flaccid paralysis of limbs, may have decerebrate rigidity, deep breathing, and poor prognosis.
Secondary intraventricular hemorrhage
mostly involves bleeding from the basal ganglia and thalamus into the subarachnoid space. In addition to headache and vomiting, there may be obvious localization signs.
Auxiliary examinations have different focuses, and
head CT is selected according to the symptoms: is the first choice examination for diagnosing cerebral hemorrhage
① CT shows high-density shadow in the acute phase.
② It can display the bleeding site, amount of bleeding, midline shift, and whether it has broken into the subarachnoid space and ventricle, which is helpful to guide treatment and judge prognosis.
③ Hematoma volume calculation method, hematoma volume = length × width × layer × π/6
Head MRI: is sensitive to cerebral hemorrhage and can clarify the location and scope of bleeding, cerebral edema and ventricular conditions.
MRI performance depends on changes in the amount of hemoglobin contained in the hematoma. This examination takes a long time and is not as simple and fast as CT, but it is worse than CT for infratentorial hemorrhage.
Cerebral angiography (DSA, MRA, CTA) can show the displacement of blood vessels, and can also find causes of cerebral aneurysms, vascular malformations, and moyamoya disease.
Lumbar puncture cerebrospinal fluid examination: The pressure of cerebrospinal fluid increases, and it is mostly uniform and bloody. When CT is unavailable, lumbar puncture can be performed with caution if the condition is not very critical and there is no obvious intracranial hypertension.
blood, urine routine , blood sugar, and electrolyte tests: helpful for differential diagnosis and understanding of the patient's systemic condition.
A clear diagnosis is the first step to success
Cerebral hemorrhage can be diagnosed in combination with the following conditions:
• Age of onset is over 50 years old with a history of hypertension.
• It usually occurs during activities or emotional excitement.
• The onset is sudden, with varying degrees of consciousness disturbance and symptoms of headache, vomiting, high intracranial pressure .
• Hemiplegia, aphasia, focal signs of NS.
• Imaging examination is the most reliable basis for diagnosing cerebral hemorrhage.
Diagnosis and differential diagnosis are indispensable

Treatment is against time and no room for error
1, acute phase
Treatment in the acute phase is to save the patient's life, reduce disability, and prevent recurrence , is a critical period of treatment.
General treatment
• In principle, treatment is performed on the spot, avoid long-distance transportation, and try to keep the patient in bed quietly.
• Keep the respiratory tract open, maintain nutrition, water and electrolyte balance, and strengthen care.
• Lowering body temperature can reduce brain metabolic rate, reduce oxygen consumption, protect brain cells, and reduce cerebral edema. Physical cooling is often used, such as ice caps, ice blankets, etc.
Dehydration reduces intracranial pressure, controls cerebral edema, and prevents brain herniation
• 20% Mannitol 125-250ml intravenous infusion once.
• Furosemide 20-40mg intravenous injection, once every 6-8 hours, or used alternately with mannitol for about a week.
• Glyceryl fructose 250ml-500ml, 1-2 times/d.
• Intravenous infusion of 50-100ml of 20% or 25% human serum albumin, 1-2 times/d, can increase colloid osmotic pressure, make dehydration last longer, and avoid hypotension.
Note: During the active phase of cerebral hemorrhage, within 6 hours after the onset, the bleeding may not have stopped, and dehydration agents should be used with caution. Mannitol used in the acute stage of cerebral hemorrhage has no effect on the bleeding brain tissue. Instead, it dehydrates the normal brain tissue and reduces the brain volume, causing secondary bleeding.
Adrenal glucocorticoids resist cerebral edema and have a slow effect on reducing intracranial pressure, so routine use is not recommended. Patients with gastrointestinal bleeding, pulmonary infection and diabetes should use it with caution or disable it.
For patients with severe cerebral edema and intracranial hypertension, when dehydration treatment is not effective, surgical decompression should be performed.
Blood pressure control
There is no unified conclusion on the standard of blood pressure control in the acute phase. It is currently believed that patients with acute cerebral hemorrhage should not lower their blood pressure too quickly and the extent of the drop should not be too large. It is more important to detect blood pressure. Corresponding measures need to be taken to deal with persistently elevated blood pressure.
First of all, attention should be paid to distinguishing between different causes of increased blood pressure, such as:
Various stimuli lead to transient and reactive increases in blood pressure: anxiety, tension, white coat effect, etc.;
Increased intracranial pressure after stroke → Elevated blood pressure
Transient reactive hypertension → Sedation
Hypertension caused by increased intracranial pressure → Actively lower intracranial pressure
People with a history of hypertension → Antihypertensive drugs, lower blood pressure slowly and steadily Pressure
How to deal with acute hypertension?
• Blood pressure of 200/120mmHg can be used for antihypertensive treatment;
• Keep blood pressure at a level slightly higher than before the onset;
• Blood pressure can be observed below 180/105mmHg, and there is no need to use antihypertensive drugs. If blood pressure continues to be too low, vasopressor drugs should be used;
• Pay attention to individual sensitivity to antihypertensive drugs.
During treatment, dehydrating agents can be used first. If the blood pressure still does not drop, it means that the increase in blood pressure may have nothing to do with high intracranial pressure, and then antihypertensive drugs can be used. When lowering blood pressure, attention should be paid to lowering blood pressure slowly and not too much. Improper blood pressure lowering can reduce cerebral perfusion pressure and aggravate tissue damage around hematoma. Usually, 10ml of 25% magnesium sulfate is injected intramuscularly or intravenously.
Surgical treatment
Purpose: to clear the hematoma, reduce intracranial pressure, and save lives. For patients with large amount of bleeding, medical treatment and continuous changes in condition, and CT confirmed that the hematoma continues to expand. Surgical treatment may be considered. There are several surgical methods: decompressive craniectomy, small bone window craniotomy to remove hematoma, minimally invasive hematoma removal, neuroendoscopic treatment, broken suction technique and simple suction, etc.
2, recovery period treatment
① As long as the vital signs are stable, rehabilitation treatment should be carried out early, and rehabilitation treatment such as exercise and language training of the paralyzed limbs should be carried out within 3 months to promote functional recovery.
② Control high blood pressure and prevent recurrence.
This article has summarized and summarized. This article basically covers the basic and clinical knowledge points of cerebral hemorrhage. The difficulty in the diagnosis and treatment of neurological diseases lies in the complex structure and physiological functions of the brain, which makes diagnosis difficult; some diseases have a sudden onset and require treatment. It is difficult; there are many factors that affect the prognosis, and recovery is difficult. I hope you will overcome difficulties and continue to make progress.
Source: Medical community
Editor: Arzt
For learning and communication only!